Introduction
Ethics of Organ transplantation stands as one of the remarkable achievements of modern medicine. The ability to replace a failing vital organ with a healthy one has transformed countless lives. However, behind this medical marvel lie complex ethical dilemmas that have challenged physicians, researchers, and policymakers. This article delves into the history, ethical concerns, and societal implications of organ transplantation.
Digital News Planet | Your Source for Thought-Provoking News.
Informed Consent in Ethics of Organ Transplantation
In organ transplantation, informed consent is a fundamental ethical precept. It refers to the process by which potential organ donors or recipients receive comprehensive information about the procedure, its risks, benefits, and alternatives. Informed consent ensures that individuals make autonomous decisions based on accurate knowledge without coercion or undue influence.
In the context of organ transplantation, obtaining informed consent involves:
- Transparent communication with living donors.
- Addressing their concerns.
- Ensuring they fully comprehend the implications of their decision.
Balancing altruism—the desire to save a life—with the potential risks to the donor’s health is at the heart of this ethical consideration. By respecting autonomy and providing clear information, the medical community strives to uphold the principles of informed consent in this life-saving practice.
The Pioneering Miracle
On December 23, 1954, Drs. Joseph Murray and John Merrill performed the first successful kidney transplant between monozygotic twins. The recipient lived another eight years, marking the dawn of the transplantation era. Yet, ethical questions emerged immediately. Dr. Murray himself grappled with the idea of taking an organ from a healthy person—a fundamental shift in medical aims. The moral landscape was further complicated by issues like obtaining kidneys, consent, compensation, and fair recipient selection1.
The Miracle of Capetown
In 1967, Dr. Christiaan Barnard achieved another miracle—the world’s first heart transplant. The ethical challenges intensified. How should organs be sourced? What about living donors—how could consent be obtained without coercion? Should unrelated donors receive compensation? And how do we define clinical death for organ harvesting? These questions echoed through medical conferences and literature, acknowledging their ethical and legal complexity1.
The Scarcity Dilemma
Regardless of the source, far fewer organs are available than patients in need. 1984, the National Organ Transplant Act was enacted in the United States. It established a task force to examine organ procurement’s ethical, social, and economic aspects. The principle of distributive justice became central—how do we allocate scarce organs fairly?
Ethical Considerations
- Informed Consent
- Obtaining consent from living donors without coercion.
- Balancing altruism with potential risks.
- Fair Allocation
- Developing transparent criteria for recipient selection.
- Ensuring equitable access to organs.
- Organ Trafficking and Commercialization
- Preventing exploitation and commodification of organs.
- Addressing the global black market.
- Dead Donor Rule
- Defining clinical death and ensuring ethical organ retrieval.
- Living Donor Protections
- Safeguarding living donors’ well-being.
- Monitoring long-term consequences.
Conclusion
The ethics of organ transplantation remain a dynamic field. As medical advancements continue, we must navigate these complexities with compassion, transparency, and a commitment to saving lives. Digital News Planet brings you this exploration of the ethical dimensions surrounding this life-saving practice.
-
What is organ transplantation?
Organ transplantation is a medical procedure where a healthy organ or tissue is surgically removed from one person (the donor) and placed into another person (the recipient) who has a failing or damaged organ. Commonly transplanted organs include the heart, kidneys, liver, lungs, and pancreas. This life-saving procedure aims to improve the recipient’s quality of life and extend their lifespan1.
-
How has organ transplantation changed in the last century?
Over the past century, significant advancements have occurred in organ transplantation. These include improved surgical techniques, better organ preservation methods, and the development of immunosuppressive drugs. These innovations have led to higher success rates, reduced rejection, and increased availability of organs for transplantation. Additionally, establishing national and international transplant networks has streamlined the process and improved patient outcomes.
-
Who is responsible for paying the cost of transplantation of a donated organ?
The expenses related to organ transplantation may be high. Many of the costs are usually covered by health insurance, including government programs like Medicare and Medicaid. However, patients may still have out-of-pocket expenses, such as copayments, deductibles, and medications. Some transplant centers also offer financial assistance programs to help alleviate the financial burden for patients and their families.
-
Why is organ transplantation challenging?
Organ transplantation presents several challenges:
Organ Shortage: There is a persistent shortage of available organs for transplantation, leading to long waiting lists.
Immunosuppression: Recipients must take immunosuppressive medications to prevent organ rejection, which can have side effects and require lifelong management.
Tissue Matching: To minimize rejection risk, finding a compatible donor-recipient match is crucial.
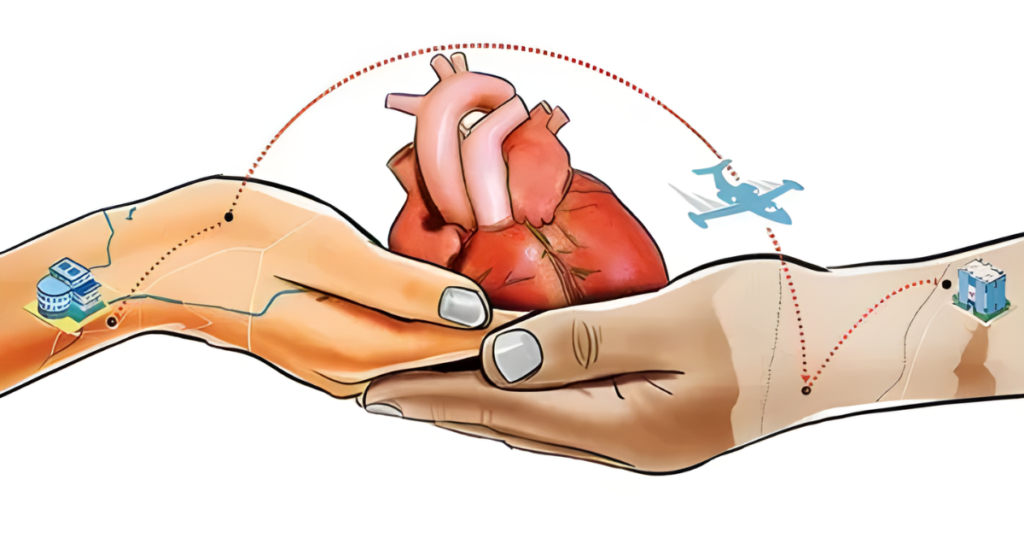
Logistics: Coordinating organ retrieval, transportation, and surgery involves complex logistics.
Ethical and Legal Considerations: Balancing the rights of donors, recipients, and society raises ethical and legal questions1. -
Why has organ transplantation changed so drastically in the last 50 years?
Several factors have contributed to the significant changes in organ transplantation over the past 50 years:
Medical Advances: Improved surgical techniques, better understanding of immunology, and effective immunosuppressive drugs.
Organ Preservation: Advances in preserving organs during transport have increased transplant success rates.
Transplant Networks: National and international networks facilitate organ sharing and allocation.
Public Awareness: Increased awareness about organ donation has led to more donors.
Research and Innovation: Ongoing research drives continuous improvement in transplantation outcomes. -
Who provides guiding principles on human organ transplantation?
The World Health Organization (WHO) offers guiding principles and policies for human organ transplantation. These guidelines address ethical, legal, and medical aspects, ensuring safe and equitable practices worldwide. Additionally, national and regional transplant organizations collaborate to establish best practices and ensure ethical organ allocation.

